What is infertility?
Infertility, whether male or female, can be defined as 'the inability of a couple to achieve conception or to bring a pregnancy to term after a year or more of regular, unprotected intercourse'.
What is the incidence of infertility worldwide?
The World Health Organization (WHO) estimates that approximately 8-10% of couples experience some form of infertility problems. On a worldwide scale, this means that 50-80 million people suffer from infertility. However, the incidence of infertility may vary from region to region.
Is infertility exclusively a female problem?
No. The incidence of infertility in men and women is almost identical. Infertility is exclusively a female problem in 30-40% of the cases and exclusively a male problem in 30-40% of the cases. Problems common to both partners are diagnosed in 10-15% of infertile couples. After thorough medical investigations, the causes of the fertility problem remain unexplained in only a minority of infertile couples (5-10%). This is called unexplained infertility. We offer total Female Infertility Treatment India
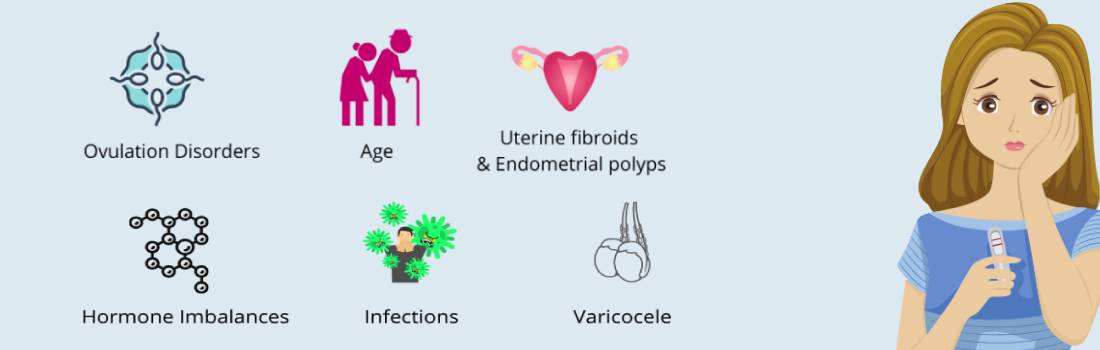
What are the most common causes of infertility?
-
The most common causes of female infertility are ovulatory disorders and anatomical abnormalities such as damaged fallopian tubes. Less frequent causes include, for example, endometriosis and hyperprolactinemia, thyroid gland related problems etc.
-
In developing countries like India, infections of the womb such as gonorrhoea, chlamydia and tuberculosis significantly contribute to infertility
-
Causes of male infertility can be divided into three main categories:
a. Sperm production disorders affecting the quality and/or the quantity of sperm.
b. Anatomical obstructions.
c. Other factors such as immunological disorders.
d. Approximately a third of all cases of male infertility can be attributed to immune or endocrine problems, as well as to a failure of the testes to respond to the hormonal stimulation triggering sperm production.
However, in a great number of cases of male infertility due to inadequate spermatogenesis (sperm production) or sperm defects, the origin of the problem still remains unexplained. -
Damaged fallopian tubes?
In the beginning In Vitro Fertilisation (IVF) was developed for patients facing infertility due to damaged fallopian tubes. Later on the indications to perform IVF were broadened with for example unexplained infertility and male infertility. Nowadays tubal damage still accounts for a large number of all IVF treatments. The main cause is infection. In developing countries such as India, the biggest culprit is Genital Tuberculosis, in which the womb of the patient is infected by the tuberculosis germ which then affects the tube leading to irreversible damage due to sexually transmitted diseases (for example Chlamydia or Gonorrhea) but complicated appendicitis or Pelvic Inflammatory Disease (PID) can also cause damaged tubes. Other causes are abdominal operations (gynecological operations, cesarean section, sterilization or other) and internal diseases like Crohn's disease. Affected patients can have fertility problems and are at risk for having a pregnancy located in the tubes (ectopic or tubal pregnancy).
-
PCOS
Polycystic ovary syndrome or shortly PCOS, is an ovulation disorder which affects 4-6% of all women. Several factors contribute to the disease. At this moment researchers think that the cause of the disease is genetic. The major features of this syndrome are irregular or no menstruation, hirsutism and acne due to high levels of male hormones, obesity (40-50%), high insulin levels with risk for developing diabetes and large polycystic ovaries shown on ultrasound. Women with PCOS usually present at fertility clinics for counseling. To increase fecundity the treatment possibilities are mostly focused on regulation of the menstrual cycle. For this, several drugs are used (Clomiphene Citrate, Bromocriptine, Gonadotrophins) and weight loss is strongly advised. In many cases the cycle will be ovulatory and regulated by these treatments. Newer oral anti diabetic drugs such as Metformin are being more frequently used to treat PCOS, with very good outcome. Alternately, one can electrocoagulate the ovarian surface using a laparoscope, especially in those women with highly elevated levels of LH hormone. If these women fail to become pregnant, they may be subjected to Gonadotropin injections, to stimulate ovulation. This may be combined with an Intrauterine insemination procedure (IUI) .Resistant cases may be treated by performing ART procedures such as IVF or ICSI
Endometriosis
Histologically identical to endometrium,the inner lining of the uterine wall is found outside the uterine cavity. Usually, endometriosis is confined to the pelvic and lower abdominal cavity; however, it has occasionally been reported to be present in other areas as well. Endometriosis is one of the most common problems that gynecologists currently face. It is one of the most complex and least understood diseases in our field and, despite many theories, we still do not have a clear understanding of the cause or of its relationship to infertility. Since this disorder is primarily a human disease and rare in other animal species, accumulation of the facts has been slow. Although endometriosis has been considered a pathological or separate disease entity, it may not be a disease at all. It may actually be the clinical manifestation of a more basic underlying disorder, such as a basic chemical or physiological abnormality that affects the tubal motility or immune system which could be responsible for the initiation or progression of endometriosis in patients with retrograde menstrual flow. By the same token, endometriosis may not be the cause of infertility, but the result of it. Further technological developments may be necessary in order for us to fully understand this problem. Endometriosis is generally diagnosed at the time of Laparoscopy. Nowadays one can treat it by performing advanced Laparoscpic surgery using Lasers, electric current and scissors. In fact, with the advent of operative Laparoscopy, very few patients need to undergo the traditional method of opening the abdomen. Endometriosis can also be controlled (if not totally cured) by using various drugs such as Danazol, GnRh analogues or progesterones. The above mentioned treatments help many patients to become pregnant. The remaining patients may have to resort to IVF or ICSI. In our unit, we have found that ICSI gives better results than IVF.
Infertility after 40
It is generally accepted that fertility decreases with age. A woman in her twenties and thirties has a 20-25% chance of a naturally occurring pregnancy, but for a woman in her early forties this possibility decreases to 5%. In IVF therapy, women over the age of 35 are seen twice as frequently compared with younger women. In fact, age is the most important factor in IVF success rates. Research has recently revealed that fertility decreases with age because of the declining quality of the woman's eggs. Although it is not possible to improve the quality of the eggs, women in their forties (and fifties and sixties) can become pregnant using techniques which can improve IVF outcome. For example, increasing the doses of drugs used to induce ovulation will increase the number of eggs that develop in a given month, thereby increasing the chance that at least one egg will be fertilized and develop into a viable pregnancy. The most consistently successful method to increase the chance of pregnancy in women with age-related infertility is egg donation from a relative or anonymous donor. To predict a woman's fertility two blood tests - FSH (Follicle Stimulating Hormone) and E-2 (Oestradiol) - can be carried out on the third day of the menstrual cycle. These assess a woman's "ovarian reserve", in other words whether she is still producing eggs and whether these are able to produce a pregnancy. The higher the FSH, the less capable a woman's eggs are of producing a pregnancy. As a woman ages, her FSH levels increase, but younger women with poor quality eggs can also have high FSH levels.
Tests that are recommended in common to evaluate your fertility
Precise recommendations concerning fertility evaluation vary depending on your current physical and fertility condition. In common, the tests that are recommended for the female partner include the below mentioned tests.
-
Anti-mullerian harmone(AMH)
-
Follicle stimulating hormone (FSH)
-
Leutinising Hormone (LH)
-
Estradiol (E2)
-
Thyroid stimulating hormone (TSH)
-
Prolactin
-
Fasting glucose
-
Screening / Virology Testing
-
Hepatitis B
-
Hepatitis C antibody
-
VDRL for Syphilis (RPR)
-
HIV Antibody 1 and 2
-
Torch Panel
-
Cervical smear
-
Type and Rh factor
-
Clomiphene Citrate Challenge Test (CCCT) is a indicative test used to provide information concerning ovarian reserve. It involves the use of a medication called clomiphene citrate (Tab.Clomid or Tab.Serophene) to be taken orally between Day 3 and Day 7. You will be asked to take two tablets of Clomiphene together at the same time every morning for five days. A set of blood tests will be done on Day 10 to compare the results with that of Day 2 hormone tests to determine your ovarian reserve
-
Hysterosalpinogram (HSG) is a radiological procedure which uses a particular dye or fluid that is placed into the uterus and fallopian tubes to check for tubal patency and uterine contour. This procedure is typically performed between Day 6 and Day 11 of a woman's menstrual cycle.
-
Hysteroscopy is a diagnostic procedure performed utilizing a hysteroscope to check if there are any fibroids and/or polyps present in the uterine cavity, and to remove them if they are found. This procedure is normally scheduled between Day 6-11 of menstrual cycle.
-
Diagnostic/ Operative Laparoscopy: All factors can be accessed in one shot. Gold standard test for female fertility. Any factors like PCOD, adhesions, subserous fibroids can be corrected.